
The COVID-19 pandemic sucks.
Now that we’ve gotten that gross clarifying understatement out of the way, let’s quickly address the title of this article. Most likely, yes, it’s quite safe to go back to the dentist. You’re feeling a little scared to get your dental work done, or to get your teeth cleaned, still, because maybe, you don’t know what has changed at your dental office to assure that you’re not going to contract the coronavirus there.
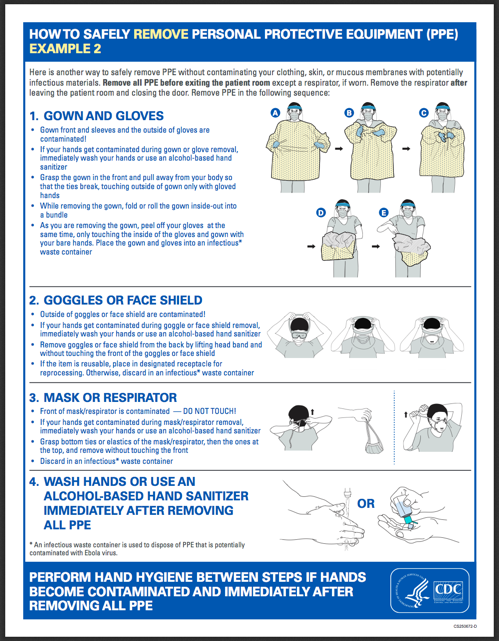
To recap the last few months, non-emergency dental care was completely shut down for a while, which had less to do with patient safety and more to do with the severe shortage of masks and gloves. Now that manufacturers, opportunists, and supply chain managers are going for the quick cash grab able to provide adequate amounts of PPE to dental practices, visiting the dentist should be no more dangerous to your health than entering any other enclosed public space.
But! There’s this annoying thing about viruses and droplets and aerosols that make dentistry quite different from visiting most medical offices.
Like everything these days, it’s complicated.
You didn’t come here for the science or the reasons that dental offices have made changes. Instead, you simply want to know whether or not your particular office is doing the right things to keep you safe, now that they have had a few months to get used to new routines.

Abundant Safety Precautions and Screening
Are you being allowed to breathe, maskless, anywhere other than in a treatment room? Surely by now you’ve had to wear a mask in public, so if you’re permitted to enter a dental practice without one, consider that your first huge red flag that they may be cutting safety corners elsewhere.
Many dental practices are having patients phone or text their arrivals in from the parking lot, making it so that there’s no stop in the reception area except for a little screening time. Furthermore, team members may check your blood oxygen saturation, along with asking a series of questions and the usual temperature-taking.
Watch for: Touchless thermometers, plexiglas barriers, pulse oximeters (finger clamps), hand sanitizer, complimentary masks.

Anonymously Mummified Clinicians
If you’re not sure who is taking care of you, congratulations! Your dentist is under there, somewhere, but is not likely to come in contact with your salivary or nasal secretions as long as those layers stay in place. Some dentists have their well-protected team members wear not just nametags, but “facetags” these days, so that you have a face to associate with each human-shaped blob that hovers near your examination chair.
Also, you may need to bring a light jacket – the exam rooms may have the ambient temperatures turned down to reduce the heat exhaustion that clinicians feel under all of that gear.
Watch for: N95 masks, scrub caps, full protective gowns, face shields, sweating complaints.

Animal-Sized Airflow Management
The rationale here: if COVID sucks, dentistry must suck harder, quite literally. If there’s no control of where infectious particles end up, aerosolized viruses are allowed to settle in place or move from room to room. Instead of letting them linger and then finding their way into your body, new large suction devices are used to pull the air directly into a filtration system that traps virus particles, making the dental environment much safer for both patients and the office staff.
Another way that dental offices are knocking down virus particles is with a powerful virus-killing fog machine. You probably won’t be able to see indications that the office is using this technology, but it never hurts to ask how they are cleaning rooms between patients.
Watch for: Large air funnels, things that look like vacuum cleaners, faint chlorine smells, HEPA purifiers

Low Aerosol Dental Treatment
In dentistry, water is utilized as a coolant to keep drills and cleaning tools from getting too hot. Unfortunately, aerosols are a big no-no right now, so there will be only the minimal amount of water used during your visits. Expect your preventive dental cleaning to be delivered quietly, with the use of hand tools only.
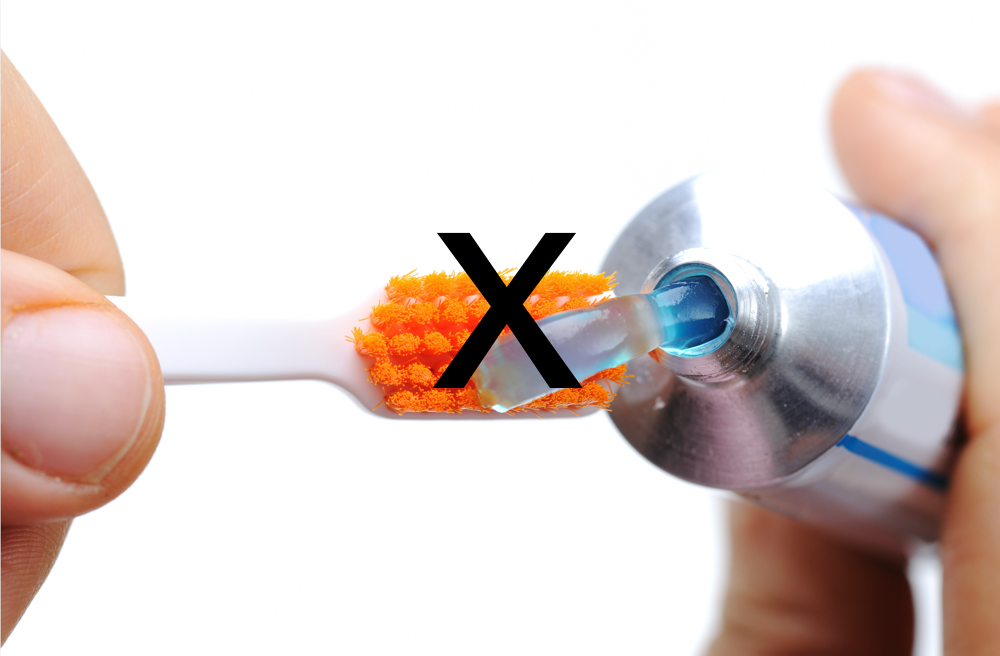
You may be asked to pre-rinse with iodine or hydrogen peroxide before opening your mouth for the first time, and even may need to hold a cup to spit in to limit the amount of automatic suctioning needed. And don’t be surprised if your hygienist doesn’t apply any grit to your teeth. Cosmetic polishing has been known to cause excessive splatter, so most state dental boards are frowning upon allowing this procedure to be performed.
Watch for: Pre-rinses, hand scraping, spit cups, tongue-grabbing high speed suction, dry mouth

Isolation and Solitary Confinement
Even with all of the precautions taken, each clinician must be very careful not to contaminate anything outside of their direct treatment area while they’re with a patient. Doctors, assistants, and dental hygienists can no longer simply move freely through the office. Instead, they are expected to stay in place until full dental care is completed.
Simple tasks like asking questions and grabbing additional equipment is now largely left to those outside of a treatment room. This is because the time and costs needed to change gowns, masks, shields, and the like have significantly increased. Dental teams are learning new ways to work together, by relying on internal collaboration software programs that give a dentist the ability to stay with one patient yet answer questions about another one via their private computer networks. If you work in a dental practice you may find the article below helpful:
Practice Communication has Changed: Isolation in the age of COVID-19
Watch for: Computerized communication systems, waiting patiently, hand signals, excessive sharing of life stories
Coronavirus has significantly altered the way that dental care is delivered, probably forever, and probably for the better. If you don’t see any differences in how care is given the next time you visit your local practice – watch out! It may mean that, in your case, when asking “is it safe to go back to the dentist?” the answer is no.

References:
ADA News: Dentistry is essential health care. https://www.ada.org/en/publications/ada-news/2020-archive/august/ada -who-guidance-recommending-delay-of-dental-care
World Health Organization: Considerations for the provision of essential oral health services in the context of COVID-19 https://www.who.int/publications/i/item/who-2019-nCoV-oral-health-2020.1
Practice Communication Has Changed: Isolation in the age of COVID-19 https://www.bluenotesoftware.com/isolation-in-the-age-of-covid19
DOCS Education – S.T.A.R. WARS: Addressing Aerosols in Dentistry https://www.docseducation.com/blog/star-wars














 A blogger since 1997, Trish Walraven, RDH, BSDH is a practicing dental hygienist and marketing manager for an indie dental software development company. She’s now concerned about the effectiveness of the mask she’s currently using in her office but continues to put it on the list of low priorities until the zombies actually come crashing into her operatory.
A blogger since 1997, Trish Walraven, RDH, BSDH is a practicing dental hygienist and marketing manager for an indie dental software development company. She’s now concerned about the effectiveness of the mask she’s currently using in her office but continues to put it on the list of low priorities until the zombies actually come crashing into her operatory.