 At first I wasn’t worried. I was probably like you, thinking this was halfway around the world, and that it was their problem.
At first I wasn’t worried. I was probably like you, thinking this was halfway around the world, and that it was their problem.
And then… it wasn’t just their problem. It became mine, too.
Now, I’m no infectious disease expert. I’m simply a dental hygienist who lives in the Dallas area, the center of the recent Ebola panic. And we should be terrified of what Ebola does to its victims. It’s scary, it’s creepy, and it’s lethal, in a super-speedy, no-time-to-say-goodbye-to-your-loved-ones zombie apocalypse way that you have probably freaked yourself out about enough already.
Instead, let’s look at how this affects us in dentistry. The question that is coming up most often between dental healthcare providers right now is “what are we supposed to do?”
The CDC offered the following Q&A reply to an American Dental Association inquiry this past September:
“Can I provide dental services to someone who has recently been in West Africa?
“CDC works with partners at ports of entry into the United States to help prevent infectious diseases, like Ebola, from being introduced and spread in the United States.
“A person infected with Ebola is not contagious until symptoms appear. Signs and symptoms of Ebola include fever (greater than 38.6°C or 101.5°F) and severe headache, muscle pain, vomiting, diarrhea, stomach pain or unexplained bleeding or bruising.
“The virus is spread through direct contact [CDC emphasis] (through broken skin or mucous membranes) with blood and body fluids (urine, feces, saliva, vomit and semen) of a person who is sick with Ebola, or with objects (like needles) that have been contaminated with the virus. Ebola is not spread through the air or by water or, in general, by food.
“Dental providers should continue to follow standard infection control procedures.”
And from the ADA website:
There is no risk of transmission of Ebola from asymptomatic infected patients. According to the ADA Division of Science and Professional Affairs, dental professionals are advised to take a medical history, including a travel history from any person with symptoms in which a viral infection is suspected. If Ebola is suspected, dental professionals may need to protect themselves with physical barriers (gowns, masks, face protection, and gloves), and contact their state or local health department.
According to the CDC, “Providers should consider Ebola in patients who develop a fever greater than 101.5 degrees Fahrenheit, severe headache, muscle pain, diarrhea, vomiting, stomach pain, or unexplained bruising or bleeding 21 days after traveling from Guinea, Liberia, Nigeria, or Sierra Leone.” Standard precautions should be used on all patients as a matter of routine.
So, did you actually READ any of the statements above? Basically, it’s saying to all dentists, hygienists, and dental assistants, move along, nothing here to see, business as usual as long as no one has been to Africa. Okay, so that used to be true.
The problem is that even though proper protocols are in place, that mean one of two things is happening to cause Ebola to infect people in the US:
1) We are not following Universal Precautions properly, or
2) Universal Precautions as we know them are inadequate.
Case in point. Today a health care worker was accused of breaching the PPE protocol because she has been now diagnosed with Ebola. The second one in our country. It could have been the other guy; you know, the deputy who went into the Ebola apartment without a Hazmat suit that ended up getting quarantined at an urgent care center up in Frisco?
Yeah, it got pretty crazy in our town last week, because he lives here. In fact, his daughter goes to school with our son. Thankfully our town responded very amazingly to him and his family at the time of crisis and we were all very relieved that it ended up being a false alarm.
So, if the problem is that we’re not following Universal Precautions, maybe then, we all need a little more muscle memory in our procedures so that we’re already doing our best if this stuff ever does become epidemic.
I know that I’m not always faithful about taking my loupes, mask, and gloves off the perfect way, every time, but you better believe that I’m going to be practicing this with chocolate syrup on my gloves the next time I’m in the office.
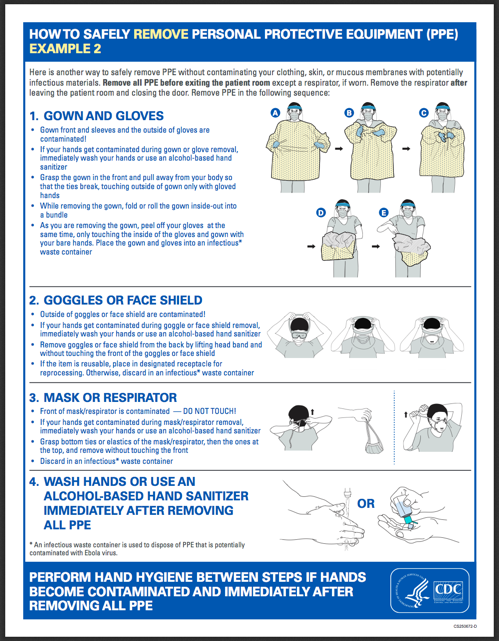
Seriously, maybe it’s time for your team to refresh themselves on how to properly remove their personal protective equipment.
Come on, who wouldn’t want to be in a room full of women (as is the case with most dental teams), passing around a bottle of Hershey’s, adding a little drizzle onto each person’s gloved hands, watching the syrup slick between their latex or nitriled-up fingers, then having them do a striptease routine in front of each other to see if they contaminate themselves?
Believe it or not, this is something that the OSHA recommends. If you’d prefer the CDC’s boring version to practice, though, you can print this PDF out instead:
As far as the other scenario? The one where the infectiousness of Ebola is far, far worse than what our sacred Universal Precautions can handle? What DO you say about that? Hey, nice knowing you, I’m changing professions now, love ya, see ya around but not here, bye?
Let’s hope then – for everyone’s sake – that we have all just been sucking at taking our gloves and masks off.
 A blogger since 1997, Trish Walraven, RDH, BSDH is a practicing dental hygienist and marketing manager for an indie dental software development company. She’s now concerned about the effectiveness of the mask she’s currently using in her office but continues to put it on the list of low priorities until the zombies actually come crashing into her operatory.
A blogger since 1997, Trish Walraven, RDH, BSDH is a practicing dental hygienist and marketing manager for an indie dental software development company. She’s now concerned about the effectiveness of the mask she’s currently using in her office but continues to put it on the list of low priorities until the zombies actually come crashing into her operatory.
UPDATE – October 16, 2014:
(Now THIS is more like it!)
ADA American Dental Association
Guidance to Dental Professionals on the Ebola Virus
A person infected with Ebola is not considered contagious until symptoms appear. Due to the virulent nature of the disease, it is highly unlikely that someone with Ebola symptoms will seek dental care when they are severely ill. However, according to the Centers for Disease Control and Prevention and the ADA Division of Science, dental professionals are advised to take a medical history, including a travel history from their patients with symptoms in which a viral infection is suspected.
Any person within 21 days of returning from the West African countries Liberia, Sierra Leone and Guinea may be at risk of having contacted persons infected with Ebola and may not exhibit symptoms. If this is the case, dental professionals are advised to delay routine dental care of the patient until 21 days have elapsed from their trip. Palliative care for serious oral health conditions, dental infections and pain can be provided if necessary after consulting with the patient’s physician and conforming to standard precautions and physical barriers.
You are advised not to treat dental patients if they have the signs and symptoms for Ebola. If a patient is feeling feverish and their travel history indicates they may be at risk of Ebola, dental professionals and staff in contact with the patient should:
• protect themselves by using standard precautions with physical barriers (gowns, masks, face protection, and gloves)
• immediately call 911 on behalf of the patient
• notify the appropriate state or local health department authorities
• ask the health department to provide you and your staff with the most up-to-date guidance on removing and disposing of potentially contaminated materials and equipment, including the physical barriers.
The Ebola virus is spread through direct contact (through broken skin or mucous membranes) with blood and body fluids (urine, feces, saliva, vomit and semen) of a person who is sick with Ebola, or with objects (like needles) that have been contaminated with the virus. Ebola is not spread through the air or by water or, in general, by food. Again, there is no reported risk of transmission of Ebola from asymptomatic infected patients.

You have a very good artlcle. I wonder if there is a set timeframe from exposure to being contagious-as in days? We shouldn’t have to see patients that have been to Africa within a certain time frame, I know this will be accused of racism or profiling or something like that but seriously I am so concerned about this runaway!
From a personal standpoint, I understand what you’re saying. But if discriminatory practices come into play, why in the world would someone admit travel to Africa if they knew they’d be denied the treatment that they’ve sought at your office?
This was the sort of scenario that instituted our Universal Precautions, where we treat every patient as though they were contagious. At the moment, there’s no reason to suspect Ebola in the general population and as long as the facts don’t change about Ebola transmission I think we’ll be good. If it’s more virulent than first disclosed, well, then, I just don’t even want to think about that yet.
The CDC website says that the incubation is from 2-21 days. The mean is 7. So someone could become sick after contact as soon as 2 or as late as 21. It also says that someone with Ebola should not have a procedure causing aerosols without an isolation room. All procedures with a cavitron or hand piece cause aerosols, and none of the ones causing aerosols are urgent enough that the risk would be worth it anyway. Therefore, I think that questioning and delaying treatment and maybe even taking temperature along with other vital signs may be a good idea for a while.
I happened to fall upon your article. What is interesting is we talk about the patients having travelled to dallas or west africa. What about your co-workers?!
In our dental office (of 21ppl) we have a hygienist that is travelling to Dallas for one week. I have never been soo scared!!..I feel like we should keep her out of the office after her return for a little bit..is this too much to ask??
I’m curious to hear others responses to this or what step they would take for prevention for themselves.
I was thinking of taking a week off when she returns so i do not have any contact with her.
Well, there are almost 7 million people who live in the greater Dallas area and no one is quarantining us unless we either lived with Duncan or treated him.
Taking a week off because someone visits Dallas is very, very extreme in my opinion. I’ll just leave it at that.
I really enjoyed reading your article. I think you managed to give your opinion without using fear mongering that I see a lot in the media.
If I’m honest, I have been burying my head in the sand when it comes to the Ebola virus. It felt like a lot of fear mongering to start off with but now I heard a couple of reports from reliable sources that make me a lot more aware of the situation.
I think it is important for health professionals like dentists to start thinking about how the threat of viruses effects general practice.
How are we supposed to disinfect our loupes? I thought the wipes were harmful to the lenses? Am I misinformed?
Hi, the loupes that we (students at dental hygiene school) purchased are cavi-wipe safe! Check with your loupe manufacturer!!
Excellent information.
My concern is that it seems that the risk to us Dental professionals is being downplayed. Although the disease is not transmitted through water or air, our instruments (hand pieces, ultrasonic scalers and Ultrasonic bath) all create an aerosol of bodily secretions mixed with blood. Are our Caviwipes and cavicide spray enough killing force to kill the disease? I’m VERY skeptical that this not something that we need to be very concerned about.
I have to agree with you. We seem to be a field of Healthcare Providers that are being ignored..Regardless of whether any of the supposed professionals on infectious disease want to admit that Ebola is airborne, we make it airborne/aerosolised with our instruments..
I’m sure we all have seen documentation of the aerosol cloud that comes from dental hand pieces/cavitrons etc.
Lets face it, We have exposed skin when we work on our patients.The masks are only protective to a certain micron level. Our hair is being covered with saliva and blood residue. We have multiple people receiving treatment in our chairs with open mouths. All things to think about.
There is no possible way to disinfect all surfaces in the dental office. I believe we are at extremely high risk not only at protecting staff, but spreading to patients. See this link: https://www.youtube.com./watch?v=0yv2UG8JzNU
Thank you to all who participate here for information and concerns.
I made an error in my post. I was meaning to say the bodily secretions are mixed with water and get into the air.
What about all traveling dentist, workers, should I ask them, if theyve been abroad lately, its not just us patients..Besides questioning doesn’t prove anything, in my office its slagger.
Ebola is not a problem at all – I got the power (like a God) to wipe out Ebola, AIDS, Malaria, TB, Colds, Flues, etc. in just a few days – I got my WVD – The Weapon of Virus Destruction – Just an exercise for a minute a day – The cure and prevention of any diseases, known on Earth for more than 2 million years – Infections, Cancers, Diabetes and Strokes – Even Tibetans don’t know how to stay absolutely healthy all the time – The price of the WVD for the whole world is 5 billion EURO/BUCKS/BP.