Bendy fake joints may not be susceptible to the bacteria introduced during dental procedures after all.
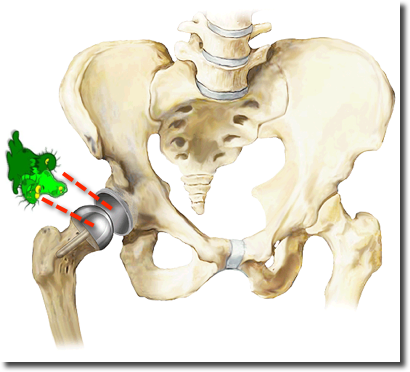
According to a systematic review of the research involving prosthetic knees and hips conducted collaboratively by the American Dental Association and the American Academy of Orthopaedic Surgeons, it was announced yesterday that there was no increase in the odds of developing a prosthetic joint infection as a result of invasive dental procedures.
This means that the Antibiotic Prophylaxis Guidelines have been updated with some sort of vague blurburbmush gabble guhg that essentially states what I’ve been saying for YEARS! When patients ask why they have to choke down those four huge amoxicillin capsules an hour before their dental visit, my answer has been something along the lines of “because it protects the dentist against liability.” This has taken some tact, of course, with explanations of how open sores in the mouth allow bacteremias every time that a toothbrush pops open a pocket and causes untold blood-squirtage- these aren’t necessarily negotiated with daily doses of doxycycline. We’ve all realized it’s good homecare, not an antibiotic, that is the key to preventing oral bacteria from getting into the bloodstream and infecting artificial joints.
Thank you, ADA, for affirming the overkill of antibiotic prophylaxis.
For the rest of the story, here’s the link:
http://www.ada.org/news/8061.aspx
_________
Update 1/2/2015:
Antibiotic premedication for joints is still not recommended.This clarification was published by the ADA yesterday:
Background. A panel of experts (the 2014 Panel) convened by the American Dental Association Council on Scientific Affairs developed an evidence-based clinical practice guideline (CPG) on the use of prophylactic antibiotics in patients with prosthetic joints who are undergoing dental procedures. This CPG is intended to clarify the “Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures: Evidence-based Guideline and Evidence Report,” which was developed and published by the American Academy of Orthopaedic Surgeons and the American Dental Association (the 2012 Panel).
Types of Studies Reviewed. The 2014 Panel based the current CPG on literature search results and direct evidence contained in the comprehensive systematic review published by the 2012 Panel, as well as the results from an updated literature search. The 2014 Panel identified 4 case-control studies.
Results. The 2014 Panel judged that the current best evidence failed to demonstrate an association between dental procedures and prosthetic joint infection (PJI). The 2014 Panel also presented information about antibiotic resistance, adverse drug reactions, and costs associated with prescribing antibiotics for PJI prophylaxis.
Practical Implications. The 2014 Panel made the following clinical recommendation: In general, for patients with prosthetic joint implants, prophylactic antibiotics are not recommended prior to dental procedures to prevent prosthetic joint infection. The practitioner and patient should consider possible clinical circumstances that may suggest the presence of a significant medical risk in providing dental care without antibiotic prophylaxis, as well as the known risks of frequent or widespread antibiotic use. As part of the evidence-based approach to care, this clinical recommendation should be integrated with the practitioner’s professional judgment and the patient’s needs and preferences.
CONCLUSIONS
Evidence fails to demonstrate an association between dental procedures and PJI or any effectiveness for antibiotic prophylaxis. Given this information in conjunction with the potential harm from antibiotic use, using antibiotics before dental procedures is not recommended to prevent PJI. Additional case-control studies are needed to increase the level of certainty in the evidence to a level higher than moderate.
The entire content can be read here: